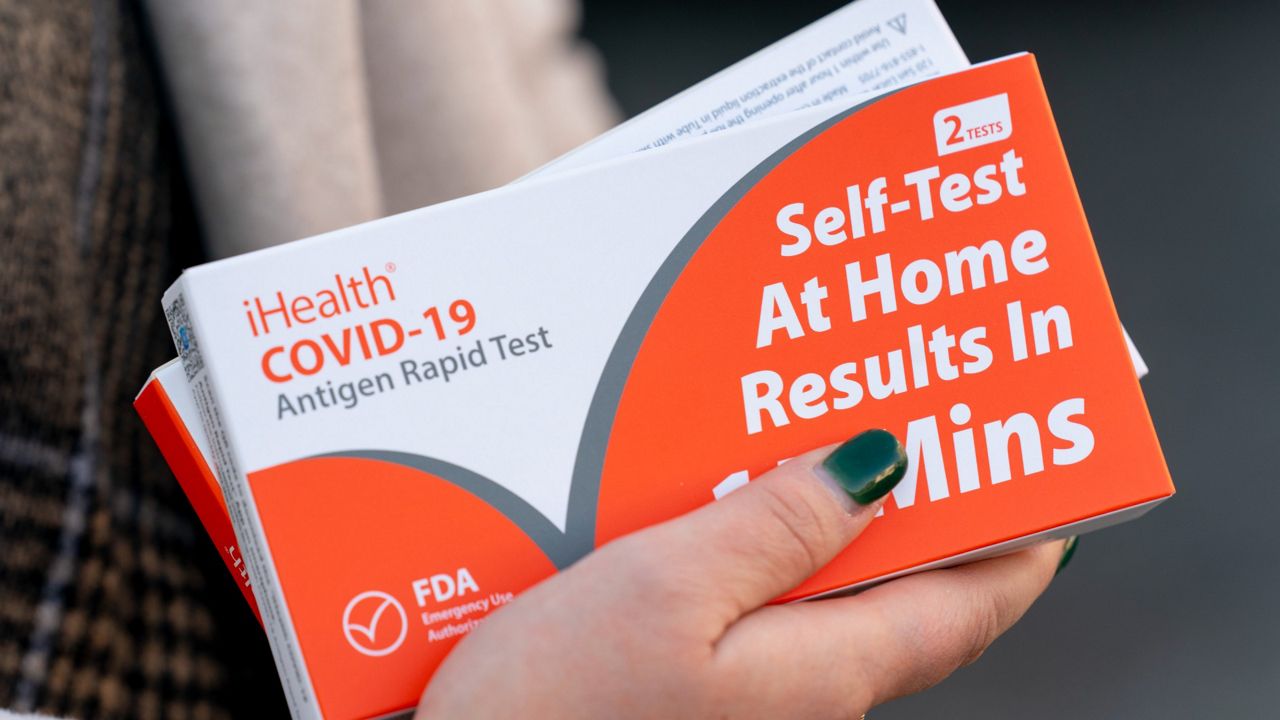
FLORIDA — Starting Jan. 15, Americans can get up to eight over-the-counter COVID tests per month that will be reimbursed through their health insurance.
What You Need To Know
- Health insurance companies will now cover up to 8 at-home tests per month
- You can bring home the test for free or submit a claim for reimbursement
- You don't need to visit your doctor or get a prescription to be eligible for the free tests
- The tests won't involve copays or be subject to any deductibles
President Joe Biden announced earlier this week that health insurance companies will have to start covering the cost of at-home COVID tests.
For example, if you go to Walgreens, you can bring home the test for free or you can submit a claim to your insurance for reimbursement.
The U.S. Department of Health says you don't need to visit your doctor or get a prescription to be eligible for the free tests, which applies to most people with private health insurance plans.
The tests won't involve copays or be subject to any deductibles.
The Biden Administration also purchased 500 million at-home COVID tests to be distributed for free across the country.
A federal website will launch Jan. 19, allowing Americans to order free, at-home tests. Those tests will usually take 7 to 12 days to ship, free of cost.
Both efforts come as many Americans continue to wait in long lines for a test or have a hard time finding them in stores.
"For us, it would be a huge burden taken off and as well as from the school because we'll actually be able to get tested on a more regular basis without having to worry so much about the financial aspect," Palm Bay resident Alejandra Escobar said.
Tests purchased before today will not be eligible for reimbursement.
The Biden Administration has also pledged to make high quality masks free and easily accessible for Americans.