ORLANDO, Fla. — An advisory committee of the Centers for Disease Control and Prevention made a recommendation in early December that has gotten few arguments:
What You Need To Know
- Orange County health official: Health care worker vaccinations will instill confidence
- Fauci: 75%-85% of US would need to get COVID-19 vaccine to get herd immunity
- But there are certain populations who have longtime mistrust in doctors, vaccines
- University of Michigan researcher proposes $50 to people to follow through on 2nd shot
- RELATED: Vaccine Reluctance: A History of Abuse Breeds Mistrust
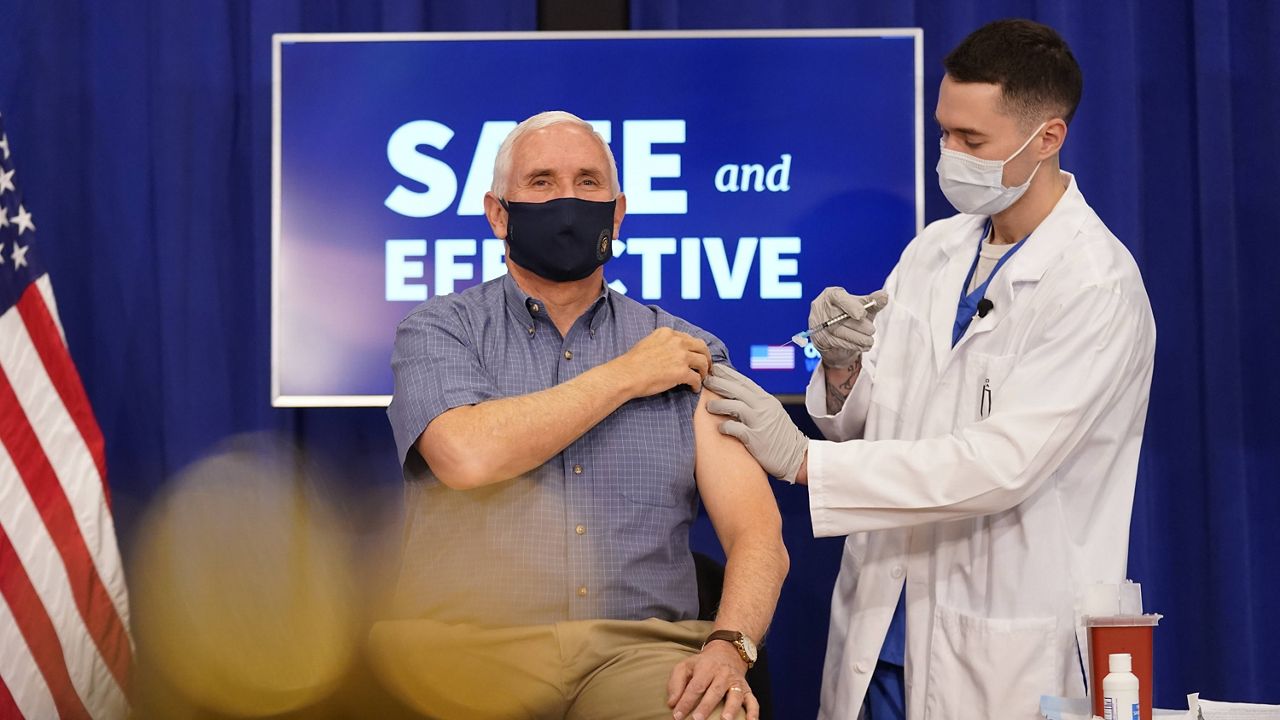
Health care personnel should receive priority in the initial phase of COVID-19 vaccinations. The committee cited a need to “preserve capacity” to treat COVID-19 patients and others.
But Dr. Raul Pino, director of the Florida Department of Health in Orange County, Florida, suggested before this week’s vaccination rollout that the panel’s decision could yield even broader benefits.
“I think the fact that health care providers are going first is going to give some level of confidence to people,” he said. “These are the people who know the value, who know the system, who know the vaccine, and they are taking it.”
Pino’s comments underscore the message that local, state, and national health officials have been emphasizing for weeks: Get the shot once it’s available, they say — and then get the required second shot.
A University of Michigan researcher and physician feels so strongly about the importance of the second shot that he proposes a $50 incentive for it.
First Things First
At issue are two critical terms: herd immunity and vaccine hesitancy.
Health officials seek herd immunity, which happens when a large percentage of a population becomes immune to a disease and makes the spread of that disease unlikely.
They don’t want vaccine hesitancy — the delay or refusal of vaccines — which hinders herd immunity.
Dr. Anthony Fauci, the nation’s top adviser on infectious diseases, told National Public Radio this week that 75% to 85% of Americans “would have to get vaccinated if you want that blanket herd immunity.”
Yet 27% of the public remains vaccine-hesitant, according to a survey released this week by KFF, an endowed nonprofit organization that focuses on national health issues. Those survey respondents said they probably or definitely would not get a COVID-19 vaccine, even if at no cost and if deemed safe — both of which are the case for the COVID-19 vaccine.
Republicans (42%), people ages 30 to 49 (36%), rural residents (35%), and Black adults (35%) emerged as the most hesitant to get vaccinated, the survey said. That compared with 26% of both white adults and Hispanic adults.
Jerry Demings, Orange County’s first African American mayor, said at a recent coronavirus news briefing that he’d take the vaccine when it’s available to him. He also pointed out “that because of the history in the United States, particularly in minority communities, there’s some distrust for vaccines in general.”
In a separate analysis, KFF reported “particularly large disparities” in COVID-19 cases and deaths for Black and American Indian/Alaska Native people and “widespread disparities in cases among Hispanic people.”
Juliette Cubanski, deputy director of KFF’s program on Medicare policy, told Spectrum News she considers it important to launch “effective outreach and messengers that resonate with specific groups of people,” including Blacks and American Indians.
Demings agreed, saying: “In order to overcome the distrust and in the reason why people will be reluctant to take the (vaccine), it would take good communication. It will take, I think, community advocacy to be able to explain why or why not an individual should take the vaccine.”
The mayor said he thinks every resident should decide for themselves whether to get vaccinated but added that “clearly, the overwhelming majority of people are going to need to take the vaccine in order to … further contain and eradicate the spread of the virus in our country.”
A Push for Participation
Health officials emphasize the safety and efficacy of the COVID vaccine. The Pfizer vaccine is 95% effective, and the coming Moderna vaccine is 94.5% effective in preventing COVID, according to studies, including at the federal level.
For full effectiveness, both vaccines require two doses a few weeks apart — which creates a second hurdle to herd immunity. Before the second dose, the Pfizer vaccine is only 52% effective, studies say.
That has sparked concern from Dr. Mark Fendrick, a physician and the director at the University of Michigan Center for Value-Based Insurance Design.
Fendrick notes behavioral and environmental challenges that might prevent people from getting a second vaccine dose. Those include logistics, politics, and reports of side effects.
To encourage more people to get the second COVID dose, he suggests a support program including transportation options, reminders of an appointment, and education about how the vaccine works.
He also proposes a $50 incentive.
“The evidence of other studies would show that $50, only on completion, would help move the needle,” Fendrick told Spectrum News.
He pointed out that employers often reward workers for participation in wellness programs. If people should be rewarded for anything, he said, it’s “to get protection from COVID’s illness and, more importantly, to be able to get our lives back.”
Cubanski, of KFF, said she sees the effectiveness of the vaccines as incentive enough. “Getting people over their initial hesitancy to get the vaccine at all, I think, is the greatest challenge that we face right now, she said.
Central Florida Efforts
Through AdventHealth, Central Florida this week joined the rest of the country in rolling out the first phase of the Pfizer vaccine.
On Tuesday, it received about 20,000 doses from Florida’s reported allotment of about 180,000 doses, and on Wednesday, it began vaccinating health care workers deemed most at risk of exposure to COVID-19.
Health experts caution that it could be into the middle of next year before the general U.S. population gets vaccinated. But officials have expressed excitement about the addition of the Moderna vaccine, which on Thursday won recommendation from a panel of independent advisers for U.S. Food and Drug Administration approval.
In addition to health care workers, the CDC prioritized vaccinations for residents who live in long-term-care facilities. Gov. Ron DeSantis this week touted Florida as the first state to begin vaccinating those residents.
"No Significant Serious Adverse Effects"
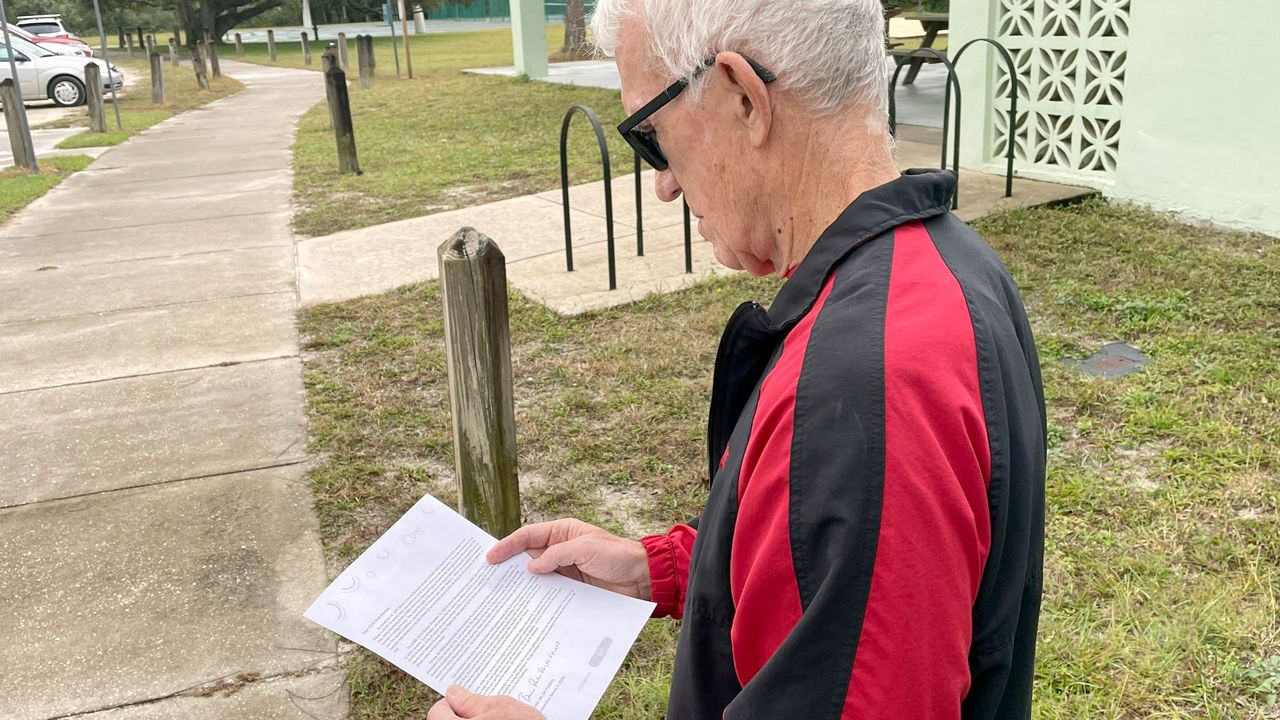
As vaccination efforts move into long-term-care facilities, health officials continue to urge residents to take the vaccinations.
Possible side effects include swelling and redness in the area of injection, plus “a bit of fatigue and some fever,” said Dr. Neil Finkler, AdventHealth’s chief medical officer for acute-care services in Orange, Seminole, and Osceola counties.
He added in a video news conference this week that the vaccine tends to produce fewer side effects in the older population than the younger population. The side effects appear slightly worse from the second shot but tend to disappear within 24 to 36 hours, he said.
“And there have been no — no — significant serious adverse effects,” he said. “I think that's really important. … If you look at the safety profile of the vaccine versus the potential risk of getting COVID and having complications, this is a very easy decision, in my opinion. And I would take the vaccine.”
Pino, the Orange County health official, added: “We are getting this chance and opportunity to give hope to seniors and to those who are affected by preexisting conditions. Take the vaccine, and be safe.”